In recent decades, a healing environment has been key within the healthcare industry as the physical environment directly affects patient care and health outcomes. With proper architecture and design, healthcare providers can perform more effectively and enable better patient safety.
Nonetheless, mere design alone cannot suffice to establish a healing environment. The hospital must integrate a seamless flow encompassing the building, its layout, and all elements in between to foster an environment of perpetual reciprocity. The alignment of care-delivery processes, workflows, and patients – as they interact with and within the building and staff – must be harmonious.
Healing Environments in Healthcare
The original concept of a healing environment was developed by Florence Nightingale whose theory of nursing called for nurses to manipulate the environment to be therapeutic. Nightingale’s theory focused on minimizing suffering and optimizing the capacity of the patient in order to recover, which included quiet, warmth, clean air, light, and a good diet.
In the 1960s, healing environments were linked with evidence-based design, creating an alignment of architecture and healthcare based on scientific design principles. At its core, the concept of healing environments in healthcare is about creating an architectural space that contributes to the patients’ healing and recovery.
Evidence-Based Design in Healthcare Architecture
Evidence-based design, a dynamic concept closely aligned with evidence-based medicine, empowers the creative process by harnessing the strength of scientific principles. By weaving together data-driven insights and cutting-edge research, it propels design decisions to new heights, ensuring a transformative impact through the architectural design.
For instance, within healthcare environments, evidence-based design exerts a significant influence on patient outcomes, encompassing factors such as length of stay, pain management, medication effectiveness, stress levels, mood enhancement, and environmental appraisals. These crucial measures serve as the yardstick to evaluate the profound effects of the physical healthcare space on an individual’s well-being. Evidence-based design follows a scientific process:
- Define evidence-based goals and objectives
- Find sources for relevant evidence
- Critically interpret relevant evidence
- Create and innovate evidence-based design concepts
- Develop a hypothesis
- Collect baseline performance measures
- Monitor implementation of design and construction
- Measure post-occupancy performance results
At the heart of evidence-based design lies the essence of basing healthcare facility planning and design decisions on an ever-expanding body of evidence. This approach seeks to attain optimal patient experiences, staff satisfaction, and operational efficiency, ensuring a harmonious synergy among all stakeholders.
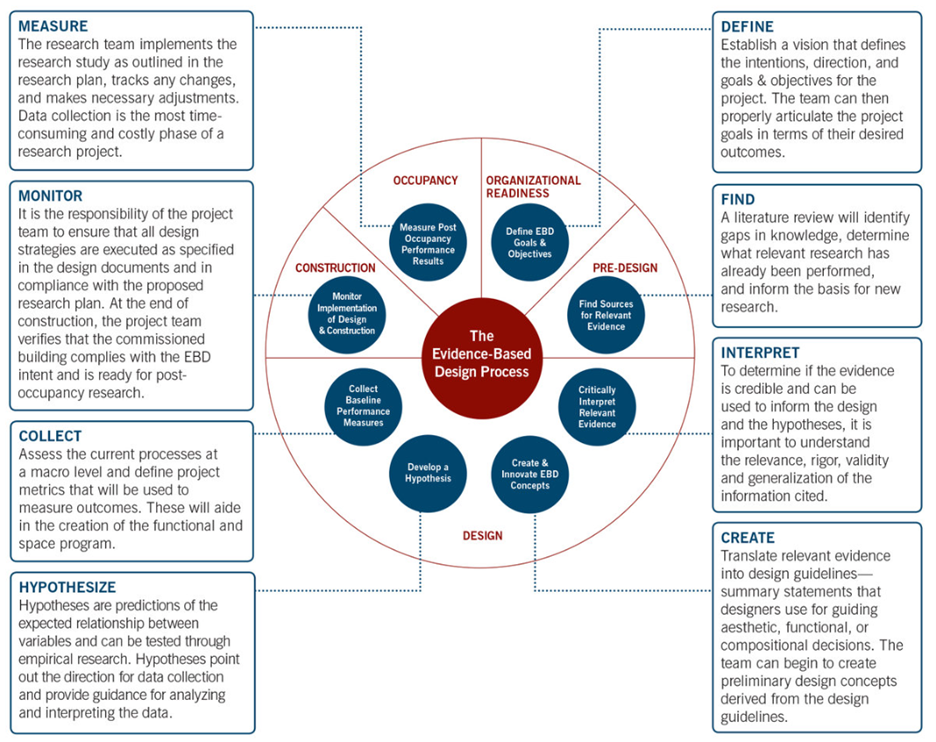
Source: The Center for Health Design
The Healing Environment with Evidence-Based Design
The healing environment is a multisensory setting that engages the physical, emotional, spiritual, and social dimensions of the individual to restore and maintain health and well-being.
The important factors include:
Single-Patient Rooms
Single-patient rooms offer a multitude of advantages, promoting shorter length-of-stays, fewer medication errors, higher occupancy rates, lower costs, lower rates of hospital-acquired infection, fewer patient transfers, increased privacy and control, less noise, fewer sleep disturbances, and higher patient satisfaction.
Noise
Noise negatively affects patients and staff, yet hospitals are known for being loud – about 65 -85dB, comparable to a noisy restaurant. These sounds come from a variety of sources, which can add to the stress. Yet, the buzzes, beeps, and alarms from equipment and the sound of footsteps on slick, easy-to-clean floors are essential to a hospital’s operation.
The road to recovery becomes obstructed in noisy environments, hindering healing, disrupting sleep, and inducing stress. To address this issue effectively, a comprehensive approach to sound control is essential. This approach encompasses the utilization of noise-attenuating materials and proper installation techniques, meticulous equipment maintenance, and strategic decision-making regarding the positioning of support spaces and equipment to mitigate noise disturbances.
Windows
Although the perception of nature’s beauty may vary from person to person, patients recovering in rooms with a pleasant view of the outdoors request less pain medication, have fewer complications, and require shorter recovery times. Similarly, for employees, access to windows and views of nature yields positive outcomes, including reduced stress levels, heightened job satisfaction, and improved overall health. The rejuvenating power of nature’s presence proves to be valuable for both patients and healthcare staff alike.
Light
Similarly, bright light, whether natural or artificial, is a key component in positive patient outcomes. Dim lighting contributes to increased depression, agitation, and sleep, disrupted circadian rhythms, and longer length of stay. With adequate sunlight, patients experience lower stress, less pain, fewer requests for pain medication, short stays – and perhaps most importantly – lower mortality.
For staff, adequate lighting that causes neither dark shadows nor bright glare is important for accuracy and effectiveness.
Access to Nature
The emotional and physiological benefits of visual and physical access to nature are undisputable. The presence of stress and negative emotions diminishes, while feelings of pleasure and well-being soar when patients have access to nature. Those who can immerse themselves in natural surroundings report lower anxiety and pain levels, reduced stress, and a speedier recovery.
Incorporating accessible gardens into healthcare settings proves to be a brilliant addition, offering both patients and staff the chance to connect with nature and enjoy its rejuvenating effects. Such spaces create a welcoming environment where individuals can interact with the natural world, fostering a sense of tranquility and contributing to the overall healing process.
Positive Distractions
As we often try to avoid distractions, some disturbances can immensely help patients to facilitate their healing process. Music, laughter, therapy pets, realistic art, flowers, trees, and water, for example, can improve mood and relieve stress for more positive interactions.
Furniture Arrangements
Furniture arrangements are essential in promoting social interactions, particularly in public settings. For example, seating that’s arranged on the perimeter of the room – like most healthcare waiting areas – and large open dining areas with banquet tables create an institutional feel and result in noisy spaces that inhibit interpersonal interactions.
Designing spaces that encourage social interactions, particularly in waiting areas, is crucial. By arranging comfortable and supportive furniture in small groupings with seating at right angles, people can interact more naturally and effortlessly. Additionally, in large dining areas, opting for smaller tables that accommodate four individuals enhances privacy and fosters social engagement.
Air Quality
Often overlooked, air quality and ventilation has more of an effect than we may think on patient and staff health. When the air quality is poor, bacteria can transmit more easily, putting patients and staff at an increased risk of hospital-acquired infections. Numerous factors can increase or decrease infection rates, including the type of air filter, direction of airflow, air pressure, air changes per hour, humidity, and ventilated system maintenance.
Careful design and maintenance of hospital HVAC systems, including the use of HEPA filtration and preventative measures during construction, are important for reducing the overall infection risk.
Flooring
Healthcare facility flooring generally falls under carpet, vinyl, and rubber options. The material’s performance is an important factor, particularly with infection control and ease of maintenance, but it can also support sound control and other desired goals.
Wayfinding
Navigating through large hospitals can be challenging for many individuals. Losing one’s sense of direction not only induces stress and embarrassment but also leads to the wastage of valuable time in healthcare settings. According to a study, confusion in a regional hospital incurred costs over $220,000, most of which was in the cost of time the staff spent giving directions.
Signage and lines on the floor aren’t enough for robust wayfinding in a hospital. A system that truly minimizes the risk of disorientation requires an integrated, coordinated system that streamlines the intersection of human behavior, environmental design, and organizational policies and practices. All these factors must work in harmony to ensure staff, patients, and visitors can navigate the environment, especially during an emergency.
Layout
In healthcare architecture, layout stands as a prominent aspect, especially concerning workstations. Workstations positioned in close proximity to patients significantly decrease a nurse’s travel time, not only for individual trips but also cumulatively over days, weeks, or months. This leads to fewer hours spent on travel and enhances overall job satisfaction among healthcare professionals. Additionally, maintaining decentralized workstations ensures essential supplies remain easily accessible, resulting in lower supply costs and improved delivery times.
Ergonomics
Both patients and staff reap the rewards of ergonomic designs. Environments designed with ergonomics in mind exhibit fewer injuries, such as falls, offering a safer space for patients. Simultaneously, the thoughtful design of patient beds, assistive equipment, and workstations results in reduced stress and fewer injuries for the healthcare staff. Embracing ergonomic principles contributes to a healthier and more efficient healthcare environment for everyone involved.
Challenges and Future Trends in Healthcare Architecture
Despite the strides made in the past decade, the healthcare architecture field continues to face mounting challenges arising from swift transformations in the healthcare industry. As we push forward, understanding and resolving these challenges will be crucial in shaping future trends in healthcare architecture.
Budget Constraints and Cost-Effective Design Solutions
In healthcare, the most critical goal is patient care, but the increasing costs of healthcare delivery across the industry are contributing to budget limitations for architectural projects. Architects must find innovative ways to create healing environments within financial constraints, such as optimizing use of space, prioritizing essential design elements that directly impact patients, and relying on sustainable materials.
Technological Advancements and Smart Healthcare Design
Healthcare is rapidly changing as a result of emerging technology like the internet of things (IoT), artificial intelligence (AI), and big data. To enhance patient care, streamline processes, and improve efficiency, this new technology needs to be incorporated into the design.
Fortunately, these same technologies can be used to enhance the capabilities of healing design. For example, IoT integration can manage environmental conditions, patient safety, and energy consumption to enhance patient experiences, promote better outcomes, and maximize investments.
Incorporating Cultural and Diversity Considerations
Healthcare is moving toward more culturally sensitive care. Healthcare providers are recognizing and respecting diverse cultural beliefs, practices, and preferences in not only the delivery of care but the design of healthcare facilities.
The integration of universal design principles plays a vital role in guaranteeing accessibility and inclusivity for individuals with disabilities. These principles encompass considerations for various aspects, such as mobility, visual impairments, and sensory sensitivities.
Additionally, inclusive communication takes center stage, incorporating features like multilingual signage and intuitive wayfinding systems that cater to people from diverse cultural backgrounds. Embracing these elements fosters a more inclusive and welcoming environment for all individuals, regardless of their abilities or cultural backgrounds.
Creating Harmony in Healthcare Facility Design
Healthcare architecture is inherently intricate, as it must accommodate a myriad of diverse requirements and standards, encompassing functional and sanitary considerations. However, taking it a step further, creating a healing environment entails more than just meeting functional needs; it aspires to elevate the overall experience for patients, staff, clinicians, and visitors alike. This approach seeks to foster an environment that not only meets essential requirements but also embraces the potential to enhance well-being and elevate the overall care experience within the healthcare facility.
At Living Style, we’re reshaping healthcare through creative, user-first design solutions and reimagining the way that healthcare facilities are designed and built to better serve patients, staff, and the community.